High transmission variants: the benefits of being proactive
There has been a lot of discussion about “variants of concern” (VOC) internationally and across Canada. One of the most important concerns is that SARS-CoV-2, the virus that causes COVID-19 and so has caused the COVID pandemic we are all facing today, has found ways to become more transmissible. We recently posted modelling work on what a higher transmission rate would look like for the number of infections. In a place like British Columbia, where cases of our usual type of COVID-19 have held steady in past weeks, a higher transmission rate means that cases would grow. Simply put, if we are balancing on the knife edge, increased transmission would put us over that edge and into exponential growth.
By now, most people following COVID-19 data have seen more than their fair share of exponential growth curves. When cases grow exponentially, there is a doubling time: first 10, then 20, then 40 and 80 cases. By the time you are at 500 there is only one doubling time left until 1000. Infectious diseases tend to grow, or shrink, exponentially, because infection doesn’t rain down randomly from the sky: people infect each other.
Imagine that we only have a few cases of a VOC, but it’s more transmissible - with each case causing 1.4 new cases on average, instead of 1, like our current type of COVID-19. With total cases resting around 400 each day, we don’t worry too much about 10 new VOC cases, and then after a month, 45, and a month later 200, but at that point the VOC has risen to reflect 30% of the total, and instead of staying constant, we have a doubling time of just two weeks.
The federal government recently introduced border measures requiring travellers to have a PCR test and to quarantine upon arrival. No doubt part of the motivation for this was to prevent continued introduction of VOCs. But that ship has left the proverbial harbour. In Ontario, for example, a recent report (p 17) found that 15.1% of cases with no known epidemiological link were the B.1.1.7 VOC. There have been multiple VOC school exposures in the Greater Vancouver area. Other provinces have similarly reported VOC cases. In most cases we do not know from public reporting when individuals with VOC COVID-19 were tested, and in what setting, and it makes a difference: not every introduction of a VOC represents established transmission. We do know that while Manitoba did identify VOC cases, later testing found very low numbers, and new travel restrictions are likely to severely limit the chance that additional VOC cases enter Manitoba. With proactive testing to screen most or all cases for VOCs, and with proactive measures when VOCs are identified, what does the modelling look like?
Here we modify and update our previous post, using a similar modelling approach, but this time, we look at what happens if VOCs start at some specified percentage of the daily reported cases and we explore the impact of more proactive measures aiming to slow the growth of VOCs. The initial values for variants come from CTV variant tracker (as of February 26), from Quebec’s INSPQ as well as from Ontario’s epidemiology report Appendix B2.
We have used low numbers for SK and MB because the CTV variant tracker showed low numbers for them (SK - 6; MB - 5) out of a total of 1428 for the country at the time, and because Manitoba has quarantine rules in place to limit the importation of variants from other parts of Canada.
We ask what happens if we continue with control measures as estimated by the model fits (blue), compared to what happens if we get a little bit “more proactive”. Here are the results:
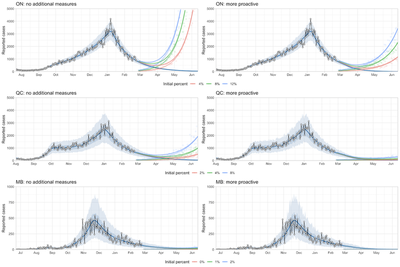
In some provinces, like Manitoba and Saskatchewan where controls on “regular” COVID-19 are strong and where VOC incidence is low, the risk that VOCs rise greatly in the next few months is low. This is due to border measures, wider testing and of course to the strength of distancing measures in place. In others, where numbers are higher and crucially where COVID-19 is in less of a steep decline, VOCs would rise steeply by May.
Being “more proactive” makes a big difference. We model “more proactive” in two ways: first, we improved control for all the COVID-19, such as would occur with stricter distancing measures (but it could be achieved with regular screening with rapid tests instead, or localized control). We also added a proactive impact of variant-specific measures. These could include prioritizing VOCs for contact tracing, mass screening of all or most contacts of cases, or other measures targeted at controlling VOCs – this must include detecting them rapidly enough to act. Together, we model detection and VOC-specific action resulting in a decrease of a further 10% decrease in transmission of VOCs.
As is always the case, models are more like flashlights than crystal balls. We use flashlights to see the path ahead - not to tell the future. When we see something we don’t like, we use that information to change the path. Here, we are not predicting that the steep rises will happen. The most likely scenario is that actions will be taken either before or when hospitalizations rise to the point where public health is concerned about capacity; the resulting distancing or other measures are not in these models.
Methods comments:
In the above figures, we illustrate what three trajectories might look like. In the previous post we looked at a large collection of possible trajectories – taking into account some uncertainty in when the VOC might become established in the community and uncertainty in how transmissible it would be. We shaded in the area that the trajectories might cover. Here, we use just one initial value (at the stated % of current cases) per colour, and just one relative transmission rate. That’s why the figures differ, compared to the previous post. The underlying model is by Anderson et al, published here. We fit it to each province’s past case count data. We then use the estimates that we get for the strength of distancing, and apply those to the new variant. We are developing this modelling further, but at this time, the method does not account for direct competition between the variant and the “regular” COVID-19. For example, with COVID-19 active cases still a very small portion of our population, we have not gone to the trouble of accounting for the same individual being exposed to both types (VOC and non-VOC) covid. The model does not yet account for the impact of vaccination. This is because vaccination, as yet and as currently planned, will not be impacting transmission for months. For our recent work on vaccination, see our recent preprint.